Understanding Medicaid Work Requirements: Implications and Insights
Introduction
Work requirements in Medicaid have emerged as a contentious topic in recent legislative discussions aimed at reducing federal Medicaid spending. A draft budget outline from Congressional Republicans proposes that Medicaid enrollees must work or actively seek employment to qualify for coverage. While the specifics of this proposal are still under development, historical data and analyses provide critical insights into the potential impacts of such requirements.
The Landscape of Medicaid Work Requirements
The concept of work requirements in Medicaid is not new. Under the Trump administration, states were encouraged to apply for Section 1115 waivers that included work and reporting requirements as conditions for Medicaid eligibility. This marked a significant shift in policy, with 13 states receiving approval for such waivers. However, the implementation faced challenges, particularly in Arkansas, where noncompliance led to 18,000 individuals losing coverage. Many of these waivers were subsequently struck down in court, and the Biden administration rescinded others, leaving Georgia as the only state currently operating under a work requirement waiver.
Current Employment Status of Medicaid Enrollees
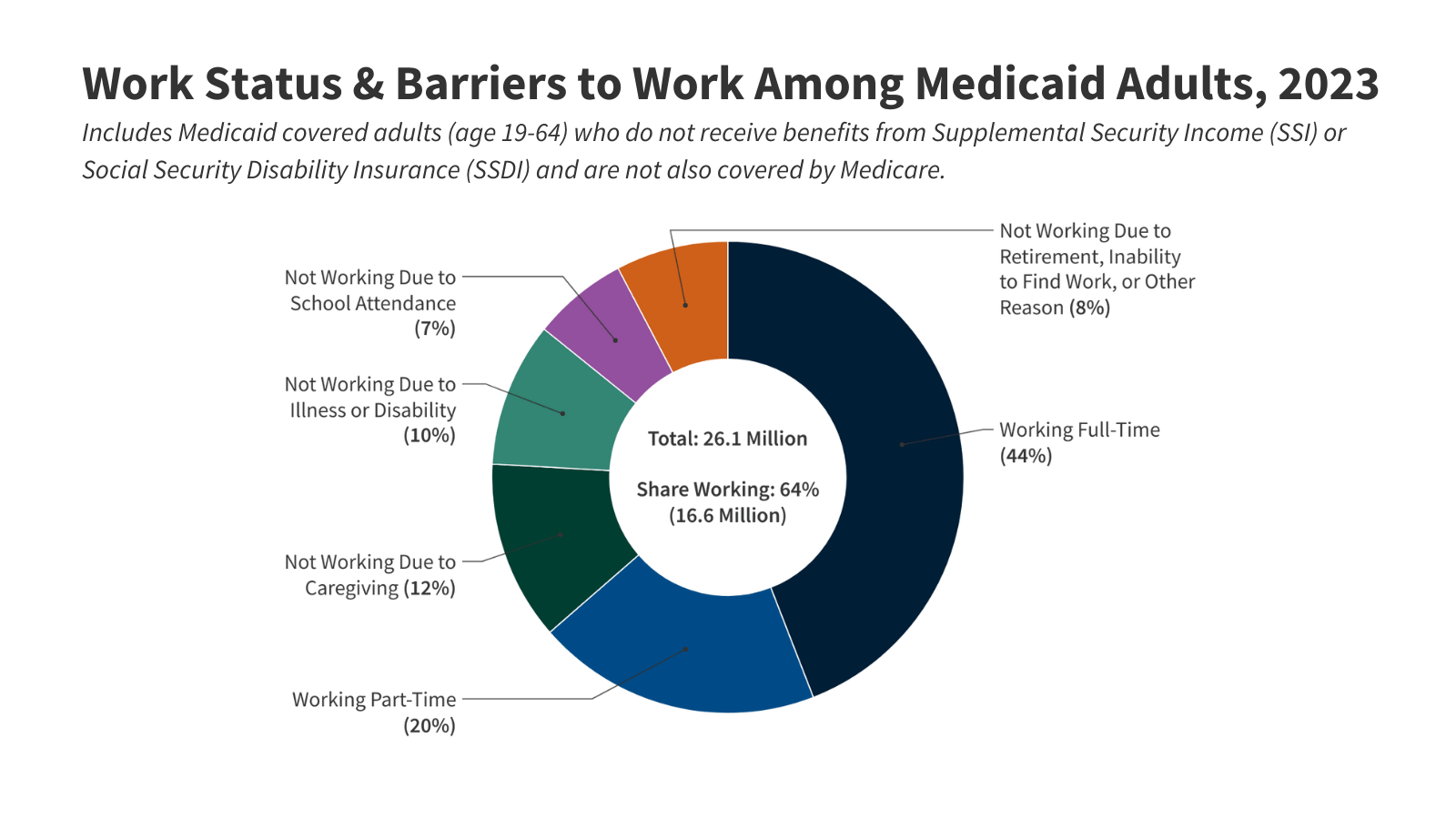
As of 2023, data reveals that nearly two-thirds of adults aged 19-64 enrolled in Medicaid are employed. Specifically, 64% work either full-time or part-time, while approximately 30% are not working due to caregiving responsibilities, illness, disability, or school attendance—reasons that previously qualified for exemptions from work requirements. This indicates that only a small percentage of Medicaid adults would be directly affected by work requirements, but many could still face risks of losing coverage due to administrative burdens and reporting complexities.
Work Status Breakdown
Among Medicaid adults under 65 who do not receive Social Security disability benefits, 92% are either working or not working due to valid exemptions. The data shows that health status, age, and education level significantly influence employment rates. For instance, individuals in excellent health and with higher education levels are more likely to be employed compared to those with disabilities or lower educational attainment.
Barriers to Employment for Medicaid Adults with Disabilities
Individuals with disabilities face unique challenges in the workforce. Approximately 32% of Medicaid enrollees with disabilities receive disability income, leaving a significant portion without financial support. Employment rates among those with disabilities are notably lower—37% compared to 68% for those without disabilities. The type and number of functional limitations also play a crucial role in employment participation, with those facing multiple disabilities struggling to find work.
Characteristics of Working Medicaid Adults
Most working Medicaid adults are employed full-time, yet many part-time workers encounter barriers that prevent them from securing full-time positions. Nearly 69% of Medicaid workers are employed full-time, but part-time workers often cite childcare issues, personal obligations, or limited job availability as reasons for their employment status.
Employment Context
A significant portion of Medicaid workers is employed by small firms, which are less likely to offer employer-sponsored health insurance. In 2023, 46% of Medicaid workers were in firms with fewer than 50 employees, where health insurance offerings are limited. This lack of access to employer-sponsored insurance underscores the importance of Medicaid for low-wage workers.
The Economic Reality for Medicaid Adults
Many Medicaid adults work in low-wage jobs that keep them eligible for Medicaid coverage. For example, an individual working full-time at the federal minimum wage earns an annual salary that falls below the Medicaid eligibility threshold in expansion states. Conversely, in non-expansion states, the median eligibility limit for parents is significantly lower, often leaving many working adults without coverage.
Conclusion
The discussion surrounding Medicaid work requirements is complex and multifaceted. While the majority of Medicaid enrollees are working, the proposed requirements could disproportionately affect those who are already facing barriers to employment. As legislative changes unfold, it is crucial to consider the implications for vulnerable populations and the administrative challenges that could arise from increased reporting requirements. Understanding the current landscape of Medicaid enrollees and their employment status is essential for informed policy-making that balances fiscal responsibility with the health needs of the population.